The Rural Surgical and Obstetrics Networks (RSON) stabilizes, supports and enhances the delivery of quality healthcare to vulnerable rural populations in British Columbia, including Indigenous populations.

What does RSON do?
RSON supports sustainable local/regional surgery programs closer to home in geographic areas served by Enhanced Surgical Skills Family Physicians (ESS FPs) or a solo General Surgeon by enhancing existing care networks shared with referral centres. Through this work, these rural surgical and obstetric networks support enhanced critical care, emergency and trauma services while also supporting closer-to-home maternity care, including vaginal birth and Caesarian section.
The local/regional RSON-supported model seeks to improve both patient and provider experiences of care by:
- understanding holistic risk and cost associated with travel so mitigation strategies can be put in place
- supporting networks of high-quality, highly effective maternity and surgical teams to provide the right care at the right time by the right providers
- supporting rural providers to practice full-scope of rural generalist medicine
- enhancing and supporting relationships between team members within the geographic network
- providing a robust evaluative framework for quantitative and qualitative metrics applied to both maternity and surgical care
- providing culturally and rurally appropriate care closer-to-home
RSON in the BMC Pregnancy and Childbirth Journal
Title: System interventions to support rural access to maternity care: an analysis of the rural surgical obstetrical networks program
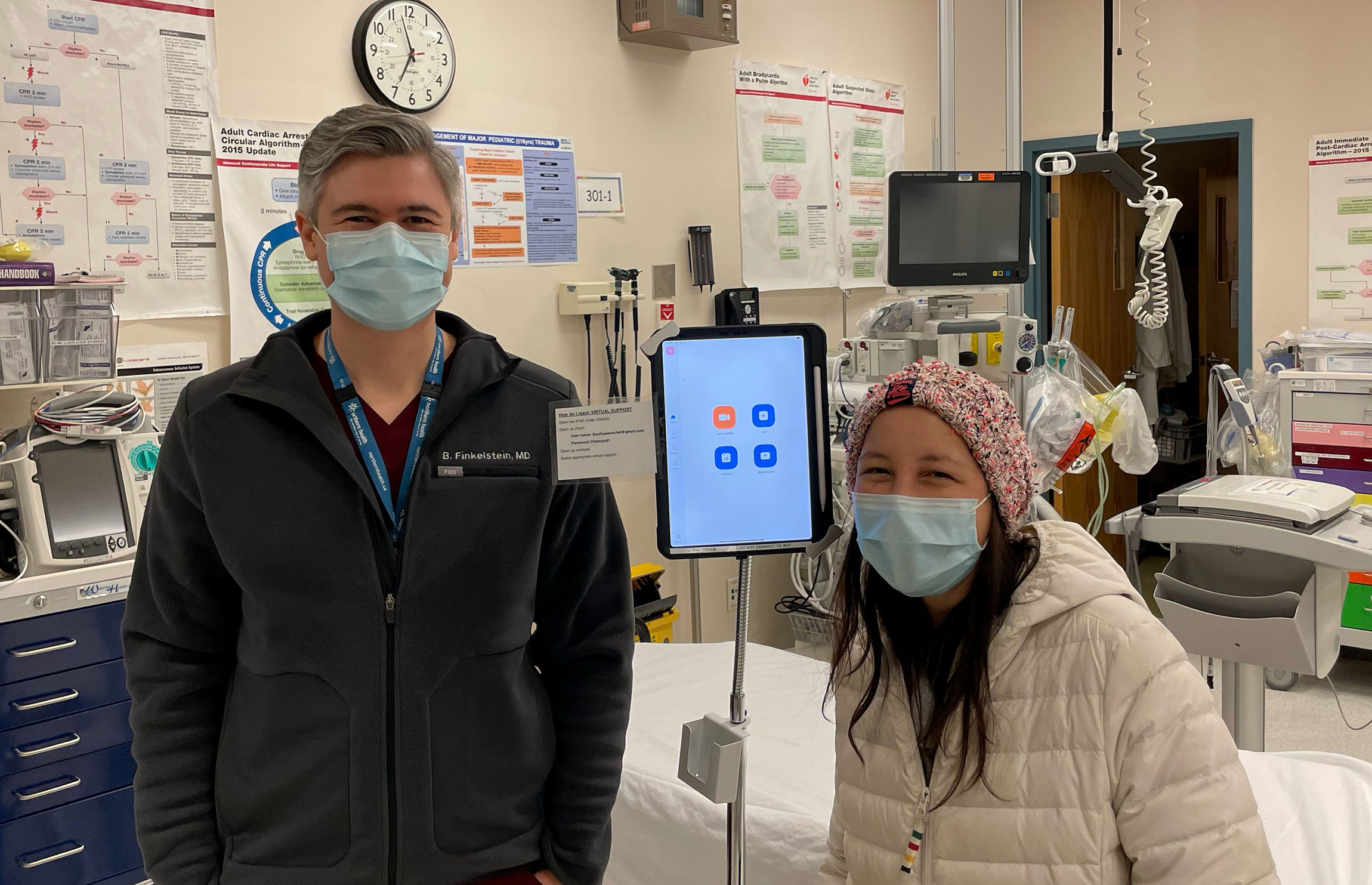
Abstract: The Rural Surgical Obstetrical Networks (RSON) project was developed in response to the persistent attrition of rural maternity services across Canada over the past two decades. While other research has demonstrated the adverse health and psychosocial consequences of losing local maternity services, this paper explores the impact of a program designed to increase the sustainability of rural services themselves, through the funding of four “pillars”: increased scope and volume, clinical coaching, continuous quality improvement (CQI) and remote presence technology.