Virtual doctors on the Real-Time Virtual Support (RTVS) Rural Urgent Doctor in-aid (RUDi) line are saving lives in remote communities.
One recent case saw a RUDi doctor use a Zoom video call to talk two nurses through a complicated, life-saving procedure.
The RUDi pathway provides clinical support 24/7 for rural providers, including nurses and nurse practitioners working on their own or in small teams in remote communities.
The video-enabled pathway is also available to rural family physicians or rural emergency physicians in need of the support of a colleague.
Providers based in remote communities simply call RUDi either over the phone or over Zoom on an iPad when they need help.
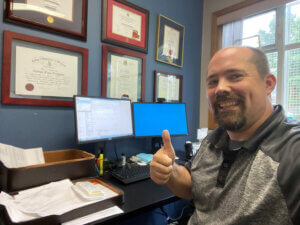
Dr. Josh Greggain, one of 35 RUDi doctors, was working a RUDi shift when he got a call from a coastal community* in the northwest of BC. The two nurses at the nursing outpost station needed help with a patient who had been brought to the station experiencing suspected Diabetic Ketoacidosis (DKA); his blood sugar was critically high, and his kidneys were failing as a result. He was in a state of near-shock, called acidosis, where his body was breaking down fat cells because he had inadequate sugar.
Josh, a rural physician with 20 years of experience who is based on Vancouver Island, ensured that the nurses had help calling the Patient Transfer Network and initiating a request for a medevac.
Josh then attempted to help the nurses stabilize the patient. He explained: “The life-saving treatment for this condition is large amounts of intravenous (IV) fluid, IV insulin infusion and IV electrolytes replacement as needed.”
The nurses on the ground attempted to start an IV—but due to the dehydration caused by DKA, they were only able to establish one single small IV.
“After several attempts to secure IV and get laboratory results, it was apparent that it was going incredibly challenging. Time was of the essence,” said Josh.
Because of cloud cover, there was no way to get a plane or helicopter to the patient to get him to a larger centre and the specialist treatment he needed, so calls were then made to the Coast Guard.
With time passing, and the patient not really improving, Josh talked to the nurses about putting in an Intraosseus (IO) line. An IO line in inserted through the bone (usually the tibia) and can be a fast and effective way to give a patient the life-saving fluid and insulin that they require. This is a critical procedure, that is used when an IV cannot be started, due to the patient’s clinical condition.
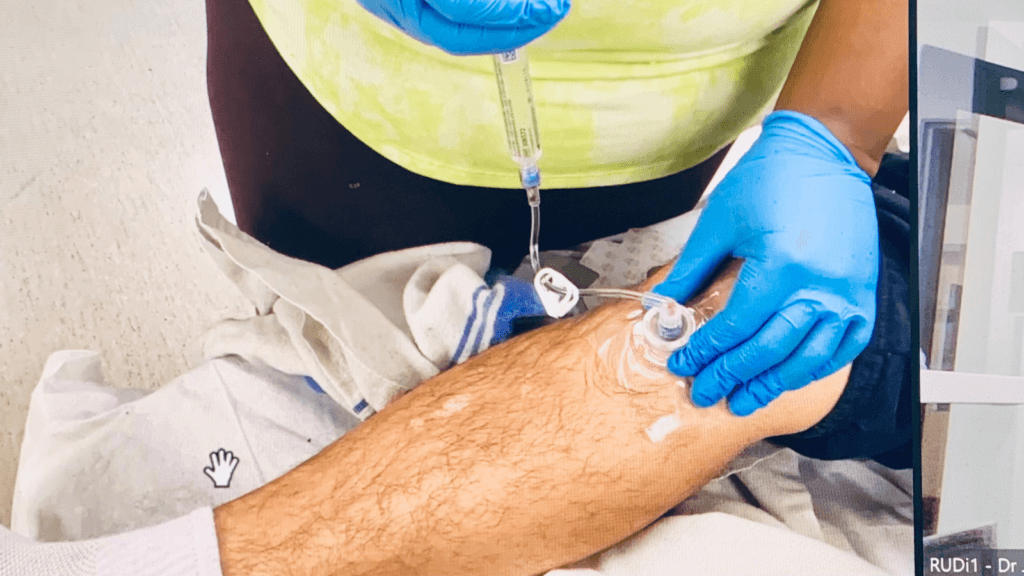
“This was the first IO line either of these brave nurses had ever put in,” said Josh. He was able to see what the nurses were doing over the iPad video call, and talk them through the process.
“We were able to run IV fluids and IV insulin to treat the patient, and prevent further deterioration while the Coast Guard was on route.”
Two hours later, the patient had improved significantly, thanks to the small IV line, and the larger IO line. The patient’s clinical state was improving, his acidosis was getting better, and his electrolytes had normalized, all thanks to the courage of the nurses who put the IO line in, with the guidance from the RUDi doctor.
“We were able to run IV fluids and IV insulin to treat the patient, and prevent further deterioration while the Coast Guard was on route.”
Josh said: “RUDi saves lives, and provides in-community nurses the support to perform life-saving procedures that they may have never done before. With the remote locations that are served, including fly-in, or boat-in only communities, this support and ability to help consult and guide from afar is nothing short of miraculous.”
As the RUDi line continues to be busy during the daytime hours, the role of our virtual medical office assistants (MOAs) is expanding. The MOAs on our team, Shannon Beer, Hayley Bennett and Karen Shepherd, will soon be operating the virtual “front door” for RUDi, from 9:00 am to 5:00 pm Monday to Friday, except during holidays, with a break from noon to 1:00 pm. The change comes into effect on March 18. This is an increase from their current hours of 10:00 am to 4:00 pm. The front door team can take down patient information and start a chart, or direct urgent calls to the RUDi physician. They can also direct pediatric calls to CHARLiE or maternity and women’s health calls to MaBAL.
If you’d like to learn more about RTVS, including how to get started using our peer pathways, visit the RTVS page.
*To protect patient privacy, the community is not being named.